In late 2010, Mary E. Beuris discovered a change in her breasts weeks after a normal mammogram. It happened that quickly: One month, she felt fine. The next, she discovered a secretion coming from one of her breasts as she slept. She brought it to the attention of her family practitioner, who referred her to me. Soon after, an imaging study detected a tiny tumor in one of Mary’s milk glands.
 Cancer survivor, Mary E. Beuris
Cancer survivor, Mary E. BeurisExperiences like Mary’s are not uncommon: Among women who are diagnosed with breast cancer, 40% detected a lump on their own, usually through a breast self-exam. That’s why it’s so important to be aware of the changes taking place in your body. The sooner you notice a change, the more quickly you can share the information with your physician. In Mary’s case, her decision to call her doctor right away saved her life.
But not all women who discover a lump share their finding with their doctor. Why? Because often, these women fear it is too late to treat the disease if they spot a symptom like this on their own. As a result, their natural inclination may be to ignore it.
If I could share one thing with my patients who are fearful of a breast cancer diagnosis, it would be this: “It’s never too late to seek care.”
Your Odds Are Better than You Think
The reasons that women put off screenings or avoid timely follow-up after detecting a lump in their breast are complex. They range from cultural beliefs to lack of familiarity with mammography screening to worries about cost or fear of bad news resulting from a screening.
What I tell my patients is that it’s important to understand that the survival rates for breast cancer are high. The five-year survival rate for localized breast cancer is 90%. That means that women who receive treatment are 90% as likely as women who don’t have cancer to live five years after receiving a diagnosis. Even in instances where the cancer has spread to nearby lymph nodes, the five-year survival rate is 85%.
 WJHL VIDEO: Dr. StanskiWomen also should know that their long-term outlook may be even better than these numbers suggest. That’s because advanced options for breast cancer detection and treatment—from 3-D mammography that pinpoints tumors in their earliest stage to medicines that attack certain types of cancer cells with precision—are strengthening outcomes, even for patients with advanced disease.
WJHL VIDEO: Dr. StanskiWomen also should know that their long-term outlook may be even better than these numbers suggest. That’s because advanced options for breast cancer detection and treatment—from 3-D mammography that pinpoints tumors in their earliest stage to medicines that attack certain types of cancer cells with precision—are strengthening outcomes, even for patients with advanced disease.
I joined Holston Medical Group in Kingsport in 2001, and at that time, I was the only female surgeon in town. That gave me a wonderful opportunity to focus on women’s health. For the past 15 years, 90% of my work has centered on treatment of breast cancer and breast-related issues. I find it extremely rewarding to support women during what can be one of the most stressful times in their lives and let them know: “I am here for you. We will navigate this journey together.”
For example, after Mary was diagnosed with breast cancer, she knew almost immediately the next steps she would take. Mary received a call from myself, telling her she had breast cancer, while at work at Abraham Lincoln Elementary School in Kingsport, where she was a teaching assistant. She cried with a friend at work. Then, as she drove home, she made up her mind about the treatment she wanted. “When I got home, I told my husband exactly what I was going to do, which was to get a double mastectomy,” Mary says. “I’m really glad I did, because it turned out there was some cancer in another area of breast tissue that hadn’t been detected.” Through it all, Mary and I worked together to review all the options and the latest research so she felt empowered to make an informed choice. I feel this is critical for my patients and it gives them a sense of control and power over a situation that can often leave them feeling powerless.
If I could share one thing with my patients who are fearful of a breast cancer diagnosis, it would be this: It’s never too late to seek care.Dr. Cheryl Stanski
When asked about her experience, Mary says “Dr. Stanski really treats the whole patient. She makes sure you have the information you need, that you understand the information, that you’re aware of the possibilities and that you feel good about your decision. I couldn’t have asked for a better doctor to guide me through this process.”
Mammograms: What to Know Before You Go
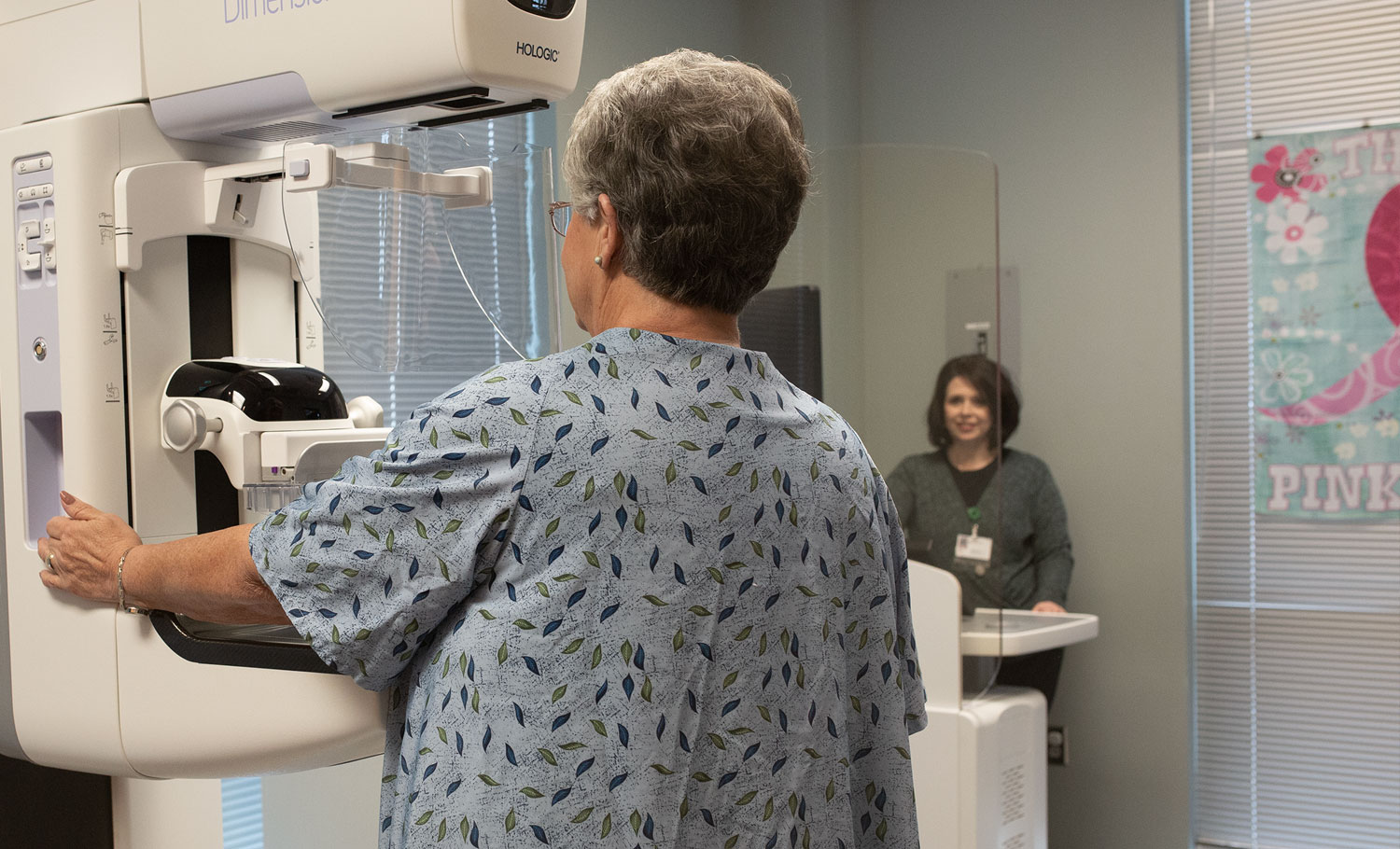
There are so many advancements in breast cancer diagnosis and treatment that have been made in the past two decades. When it comes to diagnosis, mammograms remain the best screening option for early detection. They spot existing breast cancer 90% of the time, and they can detect tumors that are too small to be felt by hand.
Wondering when you should be screened for breast cancer? The American Cancer Society suggests that women ages 45 to 54 undergo a mammogram each year. Women ages 40 to 44 may have a mammogram if they wish; those ages 55 and older may consider having a mammogram every two years or each year, depending on their preference. Women also should perform breast self-exams once a month.
Some women are hesitant to get a mammogram because the procedure is uncomfortable. But mammograms are quick—lasting 15 minutes or less—and those minutes could save your life. For example, one of my patients received a mammogram when she turned 40—and it spotted a tiny tumor at a very early stage of breast cancer. It was so small that the tumor was almost completely removed with a biopsy before we performed surgery to ensure there were no traces of cancer left. Now, she’s done with treatment. She didn’t have to go through chemotherapy because the mammogram spotted the cancer at such an early stage. It’s an example of how a regular mammogram not only can save your life, but also minimize breast cancer treatment.
If you’re concerned about the level of discomfort you might experience during a mammogram, try these tricks:
- Take an aspirin before your appointment.
- Tell the technologist that your breasts are sensitive so the technologist can take extra care during the exam to protect your comfort.
- If you are still menstruating, try not to schedule an appointment the week before your period.
One question that I am often asked by patients at HMG is, “Should I get a traditional mammogram or a 3-D mammogram?” Women who have a family history of breast cancer or who have dense breast tissue should consider 3-D mammography ultrasound, which provides amazing clarity in imaging, detecting tumors that might be obscured by dense breast tissue. However, all women could benefit from 3-D mammography. If you can afford to pay a little more out of pocket for 3-D mammography, I recommend doing so.
The Right Relationship Can Save Your Life
At HMG, we strongly believe in the power of a positive physician-patient relationship in supporting good health. I’m proud of the relationships I’ve built with women in this community over the past two decades, and I’m excited about the advancements we’ve seen locally in breast cancer diagnosis and treatment.
If you’re concerned about your risk for breast cancer, or if you have questions regarding mammography, help is just a phone call away. Contact me today at our Kingsport office at 423-392-6265.
Our Offices:
- Bristol - HMG Outpatient Diagnostic Center at Sapling Grove
- Duffield - HMG Outpatient Diagnostic Center at Duffield
- Johnson City - HMG Outpatient Diagnostic Center at Johnson City
- Kingsport - HMG Outpatient Diagnostic Center at Meadowview




